In humanitarian contexts, negotiating makes access to populations, medical interventions, and life-saving support possible.
As we explore the challenges, best practices, and insights gathered from the members of our community of practice, we hope you will gain valuable perspectives on how to navigate this critical field.
Let’s dig in.
What do humanitarian healthcare workers negotiate for?
As a healthcare professional working in humanitarian settings, you might ask yourself: do I negotiate?
And if that’s the case, what exactly do I negotiate for?
Let’s go back to the basics and define what a humanitarian negotiation is.
According to the CCHN Field Manual, a humanitarian negotiation is any interaction between humanitarian personnel and an interlocutor to:
- establish and maintain the presence of a humanitarian organisation in a crisis environment (conflicts, disasters, migration flows, epidemics…),
- ensure humanitarian access to people in need, and
- provide protection and assistance.
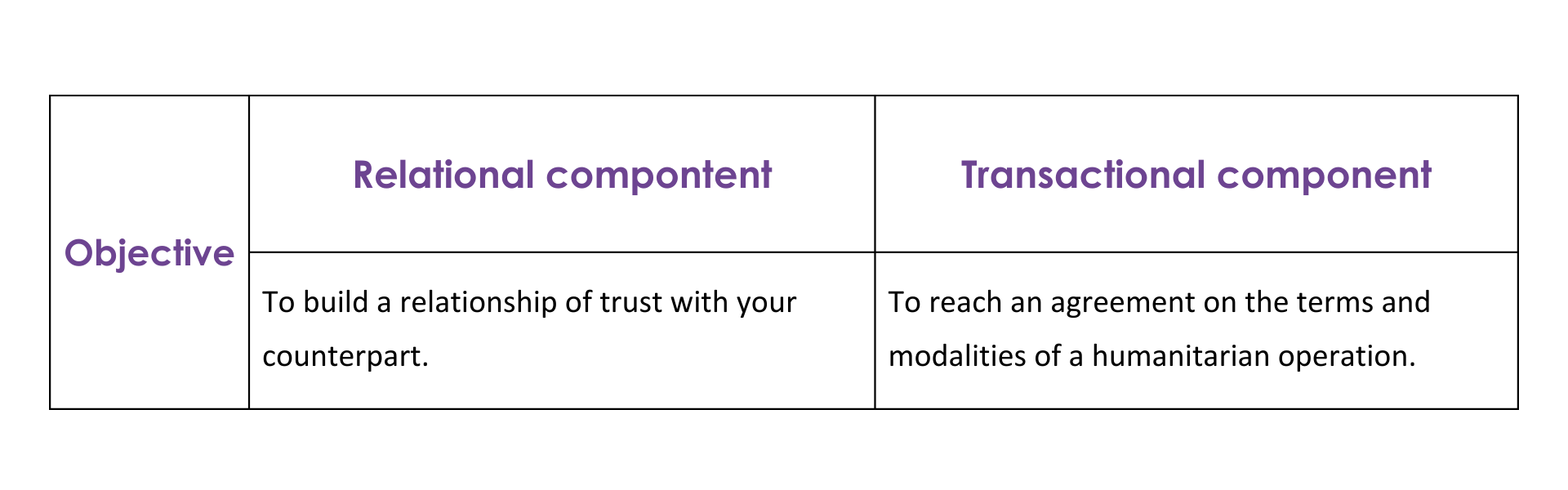
Remember: humanitarian negotiations have a relational component, focused on building an ongoing relationship of trust with counterparts, and a transactional component, focused on establishing and agreeing on the specific terms and logistics of humanitarian operations.
Therefore, as a humanitarian healthcare worker, you might think of ‘healthcare negotiations’ as any interaction with an interlocutor (like the Ministry of Health, local health authorities, non-state armed groups and even patients) to reach a compromise upon:
- The provision of health services to populations in need.
- The modalities of health interventions and the protocols or guidelines you will follow.
- The presence and acceptance of your organisation.
- The protection of medical missions, by mitigating or reducing threats.
- Day-to-day negotiations with patients, community leaders, and families of patients.
Of course, all while staying safe.
What characterises healthcare negotiations?
Healthcare negotiations differ from broader humanitarian negotiations in several aspects.
When conflicts escalate or a disaster hits, healthcare personnel operate under immense pressure.
Healthcare negotiations aren’t about how many days a distribution will take, but rather how many hours or even minutes injured or ill people may have before they lose their lives.
Hindered access to people in need of assistance or people who can’t access the timely care they need only adds to the urgency of the situation.
Working in humanitarian settings also means working within health systems with limited capacity or even damaged infrastructure, for instance when supplies can’t reach hospitals because roads are damaged.
Health negotiations not only focus on how a medical intervention will be carried out and its life-and-death outcomes, but they also involve working directly with communities and explaining the “why and how” of health campaigns managed by humanitarian professionals.
In sum, negotiating health services in crisis is an artful dance between compromise on the one hand and adherence to humanitarian principles and other normative frameworks, such as international humanitarian law, on the other. It is a relationship that requires trust, an open mind, and being adaptable.
What makes negotiating health care in emergencies challenging?
Today, humanitarians operate in constantly shifting, increasingly intricate and insecure environments. If you are a humanitarian health worker, this probably resonates with you.
Members of the CCHN community of practice shared that the protective feeling they used to have when carrying out humanitarian work, particularly medical missions, has diminished. Unfortunately, examples of hospitals, clinics and ambulances being attacked in the last few years (or months) abound.
So why is negotiating health care in emergencies becoming more challenging?
-
Assertive governments and bureaucratic and administrative impediments
Governments and health authorities are perceived to have become more assertive, sometimes intentionally introducing bureaucratic and administrative impediments that challenge swift and coordinated health emergency response processes.
For instance, they can deliberately create hurdles to the importation of drugs and medical equipment, limit humanitarians’ movement, or add barriers to staff recruitment. In many humanitarian operating environments, these obstacles may be intentional, used to control and restrict humanitarian action, while in other instances they can be the result of a lack of capacity or dysfunctional governance mechanisms.
-
Engaging with non-state armed groups
Access to areas affected by conflict or disasters often requires engaging with non-state armed groups.
However, national legal frameworks, counter-terrorism laws and sanctions often impede interactions with these actors, requiring careful explanations of the organisation’s mandate and humanitarian principles.
Humanitarian staff, and most particularly national ones, also risk being perceived as “disloyal” or “traitors” to the government by the national authorities.
-
Politicisation of health
Humanitarian health actors operate in increasingly politically charged environments. Access may be granted or restricted by forces in control of territories and blocking the provision of life-saving medical assistance is sometimes used as a weapon.
Unfortunately, being a humanitarian today doesn’t offer the same protection as before and some parties to the conflict might see unlawful targeting of medical missions as legitimate or justified.
-
Misinformation and hate speech
Misinformation, disinformation, and hate speech impact humanitarian work. Social media channels can amplify negative messages about a humanitarian operation, for example spreading a rumour that healthcare workers plan to kill or sterilise the local community. In these cases, community-based approaches and disseminating accurate information (preferably before a communication crisis hits) are crucial.
What are some negotiation strategies you can use when negotiating healthcare?
Here are seven practical tips shared by humanitarian workers with extensive experience in humanitarian health missions.
1. Aim to build a relationship
Humanitarian negotiations are first and foremost a relationship that requires trust-building, an open mind, and flexibility. This is the basis for your negotiation.
How do you build this relationship and gain your counterpart’s trust?
- Regularly engage with your counterpart. Call them, text them or email them, or take the opportunity of a face-to-face meeting to have informal conversations.
- Keep a humble and curious attitude. Try to see beyond official titles and positions and get to know your counterpart, their story and interests. Your counterpart could be someone who has also been affected by the conflict.
- Accept that they (most likely) have a different position. Ask open questions to explore their reasoning. What motivates them? What are their imperatives? What goals could you potentially have in common?
Remember, your counterpart is just as human as you are.
2. Understand your context and the local culture (including around health)
Every negotiation occurs in a unique context with its own culture and customs. Norms around the way health is regarded vary greatly between cultures.
Try to get as much information as possible about the social, political, and even religious aspects of illness and health in the context where you work.
This is crucial to engage communities effectively and develop culturally appropriate interventions. Some organisations even recruit health anthropologists, as it happened during the Ebola epidemic in West Africa.
Ultimately, being informed about your local context and its perception of health and illness will help you reach a more sustainable outcome.
3. Have a clear negotiation objective and build towards it, in milestones
Think back to what a humanitarian negotiation is. You can negotiate for acceptance, access and implementation. Achieving this will require compromises and finding a mutual agreement with your counterpart.
But first, what is your objective? In the ideal world, what would you like to achieve with your negotiation?
An objective might not be easily achievable, but it will guide you in establishing small milestones to work towards it.
For example, you know that the country you are working in is suspicious of anything related to its former colonial power, including its citizens. In an ideal world, you may wish to involve your most capable and knowledgeable staff in a particular humanitarian operation without worrying about their nationality.
Once you formulated your ideal outcome, try to adapt it to the reality in front of you.
Are there any concessions you are willing to make?
For instance, after some reflection, you decide you can accommodate your counterpart’s request and hire staff from other nationalities which do not include the former colonial power.
4. Have clear red lines
Negotiating health outcomes in a crisis involves navigating complex circumstances, all while upholding the humanitarian principles.
Establishing clear ‘red lines’ – non-negotiable boundaries – as a team and organisation allows you to sustain the integrity of your mission and the dignity of those you serve.
For instance, consider you are negotiating access to a besieged area to provide critical medical aid.
While you may need to make certain concessions, your negotiation ‘red line’ could be the impartiality of the services.
Your organisation’s policy doesn’t allow you to favour one group over another based on the demands of those controlling access.
Following the impartiality principle ensures that assistance remains accessible to all who need it, regardless of their political, ethnic, or religious affiliations.
By respecting this red line, you also guarantee your own and your colleague’s safety by showing you are not siding with any party to the conflict and potentially being targeted by one of the parties.
5. Acknowledge the political nature of healthcare negotiations
By nature, contexts affected by conflict are politically loaded and influenced by decisions removed from the realities on the ground.
It’s important to remember that although medical care might seem distant from politics, healthcare emergencies in humanitarian contexts are not.
According to the CCHN Field Manual, humanitarian negotiations can move between three levels: the political, the professional and the technical.
Being aware of this framework can help you understand on which level your counterpart feels more leverage or might be using strategically to their advantage, as well as the level on which you want to focus.
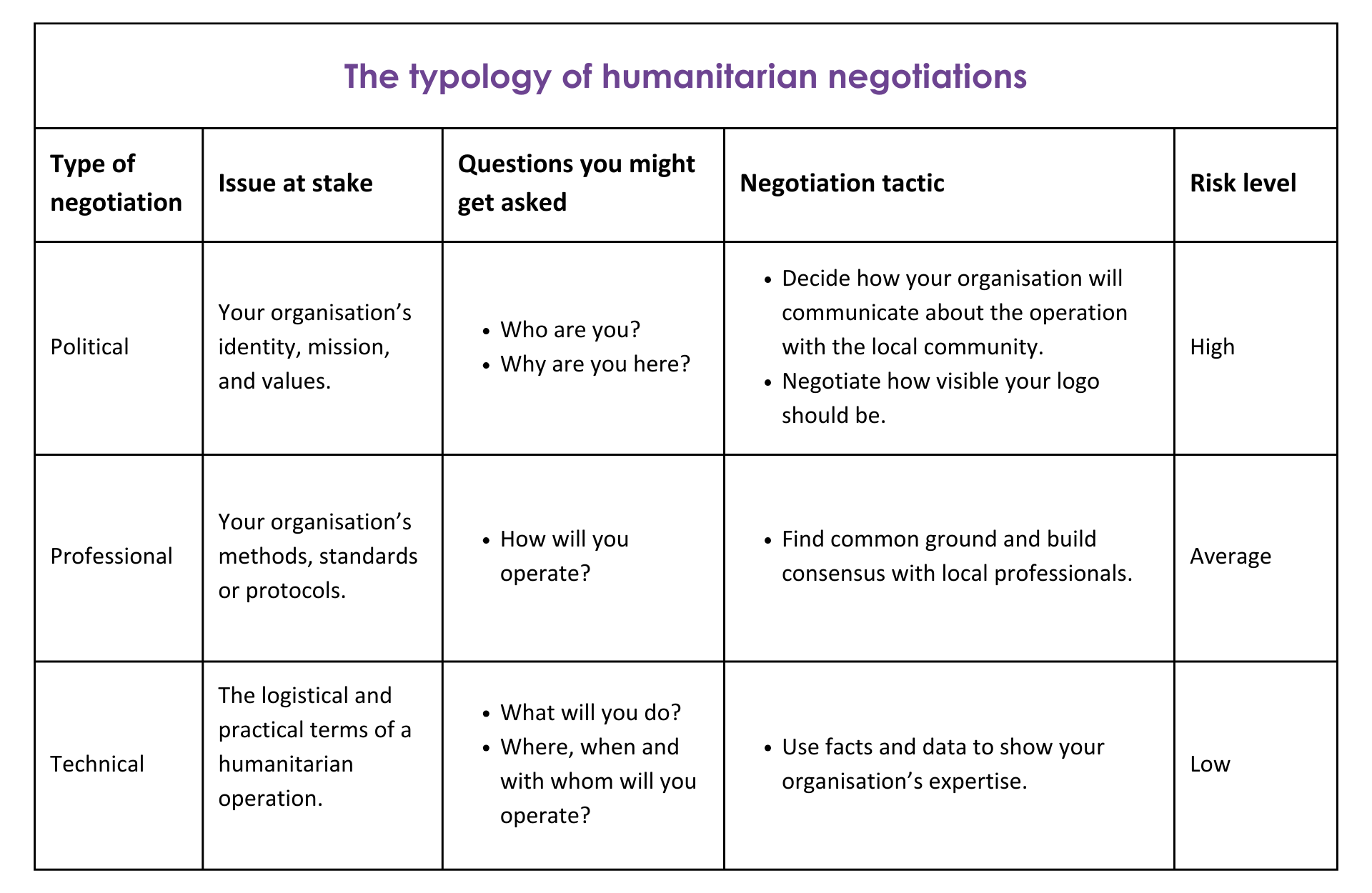
For instance, a counterpart could politicise the discussion by asking: “By the way, tell me again, why are you here and who are you?”
In the same way, you could avoid political pitfalls by asking: “How do you think we could work together and provide the necessary assistance to the population in need of support?”
Use this negotiation tactic to draw the conversation to the level where you feel more comfortable.
6. Monitor local perception
Once you start implementing your operation, it’s fundamental to monitor how it’s received.
How do local communities perceive your work?
Are they satisfied, frustrated, or suspicious about the vaccination campaign you’re leading?
Experienced humanitarian practitioners shared that often, the more concrete and tangible the assistance, the more positive the perception. But when it comes to health interventions, people can be weary of medical supplies or treatments they aren’t familiar with. Expect communities to be suspicious and help them understand the benefits of your intervention.
Being attuned to communities’ sentiments can help you understand their pain points and find ways of addressing them (if possible), which will in turn build your organisation’s legitimacy.
Check out a tool we developed to handle tense conversations with an example of how to address a father’s concern about his child getting vaccinated.
7. Negotiate as a team
Negotiation teams are composed of different levels of expertise and skills, which can be leveraged depending on the issue you are preparing to negotiate.
Humanitarian health operations are multifaceted.
You can negotiate acceptance of your organisation’s mandate or the importance of its intervention to prevent and respond to an outbreak (as in a ‘political’ negotiation).
You could also negotiate with public health authorities about importing certain drugs and medical equipment which are not available on the market (as in a ‘professional’ negotiation).
It could be that you’re simply negotiating the vaccination campaign plan in a refugee camp (as in a ‘technical’ negotiation).
At each level, or phase, you need to identify the right person to lead the negotiation.
A way to do this is to use the CCHN’s ‘legitimacy’ negotiation tool, which takes into account five sources of legitimacy:
- The institutional mission and reputation of your organisation.
- Your competence on a specific topic.
- Your personal features (age, gender, religion, nationality, etc.).
- Your capacity to adapt to changing circumstances.
- Your connections with networks of influence.
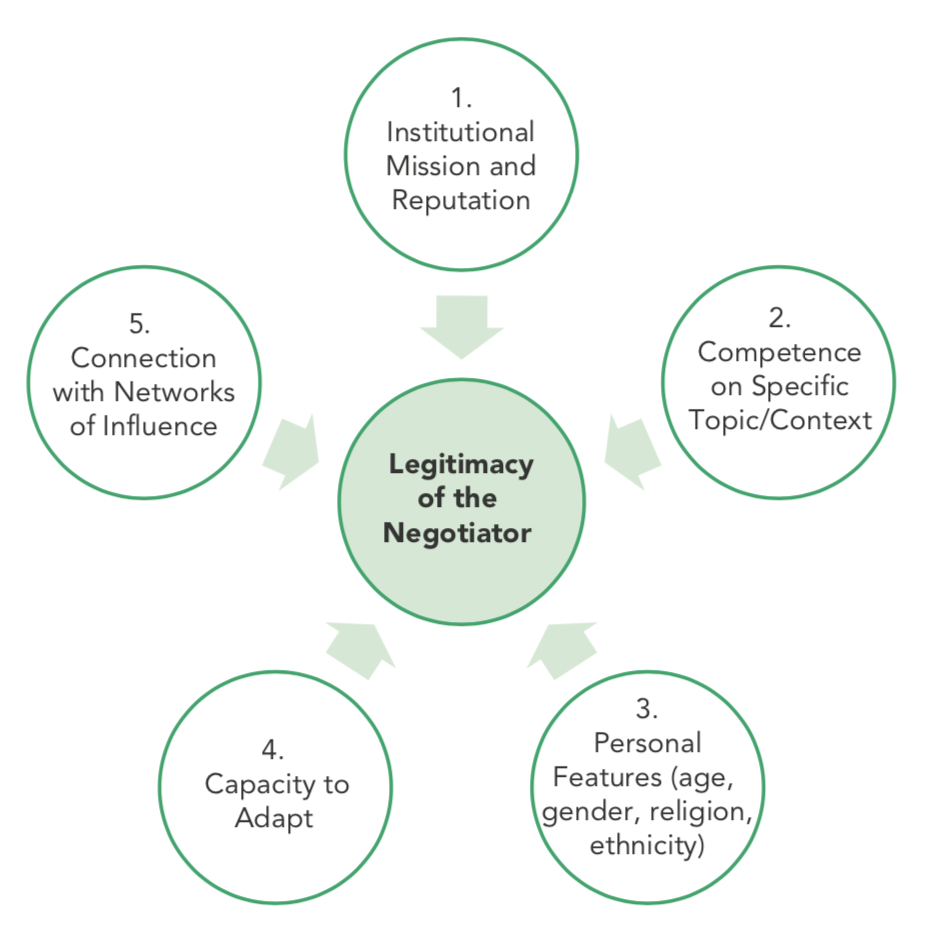
Based on the negotiation objective, your counterpart and type of negotiation, who is the best person to lead the conversation?
Remember...
Healthcare negotiations differ from broader humanitarian negotiations.
Negotiating healthcare issues in humanitarian contexts is a delicate matter that involves life-or-death situations and culturally sensitive conversations.
On top of that, negotiating healthcare in humanitarian settings is becoming increasingly challenging.
We hope the strategies shared by experienced humanitarian negotiators will prove useful for your work.
Good luck!